- You suffer, or have suffered from anemia and the solutions offered by your chosen health care professional are/ were limited to iron tablets
- You are pregnant or have just given birth and wish to find proactive ways to avoid letting your iron levels fall into anemic range
- You have been diagnosed with an inflammatory and/ or autoimmune disease which causes iron stores depletion
- Veggie or vegan and you’re worried about an increased risk of iron deficiency
If you recognise yourself among these scenarios, then this little piece is for you.
You reading this tells me you’re interested in preventing anemia; you might already know about the importance of certain nutrients such as B6, folate (B9), B12 and iron. If it’s not the case, you might find reading my piece “Anemia 101” interesting.
So, “sunshine vitamin” and iron metabolism :: what’s the deal?
Recent studies suggest ::
- Vitamin D plays a role in diminishing molecules that work to promote inflammation (cytokines, small proteins involved signaling where/ when an inflammatory reaction is needed)
- It acts as a suppressing agent of hepcidin; hepcidin being the CHIEF hormone of iron metabolism regulation
These 2 factors act in a favorable way on iron bioavailability in the human organism1 and support its equilibrium.

Hepcidin
Hepcidin, rarely discussed when “iron stores and utilisation management” is addressed in mainstream media, can be summed up like this ::
- A hormone that is produced in the liver and secreted into blood circulation.
- It acts as a NEGATIVE regulator of iron absorption and recycling.
- i.e. :: it controls transporters (ferroportin) that allow iron to travel from cells –> to plasma.
- It’s role :: inhibit iron absorption when its concentration in the body is optimal in order to avoid excesses that would throw the body off balance
- Inflammation, infections and accumulation of iron in tissues increase hepcidin production.
- During an infection, this protection mechanism triggered by pro-inflammatory molecules works to deprive invading organisms of iron in order to prevent their growth.
- However, in a chronic inflammatory state*, this process that aims to reduce available/ circulation iron can bring about “shortages” in the production of hemoglobin and red blood cells which can lead to anemia.
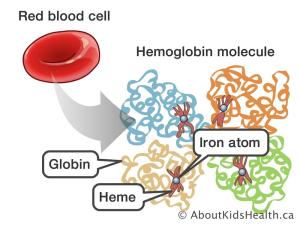
- NO iron :: NO hemoglobin. Iron is an important component of the hemoglobin molecule.
- Inadequate production of hemoglobin translates to insufficient oxygen transport to the organs that need it.
*Obesity is considered a chronic inflammatory stateA.
Iron depletion can range from asymptomatic to debilitating. Find a list of symptoms here.
Vitamin D plays a supporting role in the production of red blood cells and hemoglobin
In a normal situation :: after a meal, as required by the body, a certain proportion of ingested iron is absorbed in the duodenum.
In an individual with a smooth operating constitution, iron is stored in the liver, to be used when needed and ultimately, recycled.
When red blood cells have reached the end of their programmed “life”, which is about 120days, they’re broken down into their various components (mainly globin, heme and iron). Iron is either stored or returned to circulation where it can reach bone marrow and be used in red blood cell production once again.
An inflammatory state (characterised by IL-6 et IL-1β) triggers the liver into producing more and more hepcidin. Hepcidin rising concentrations prevents iron stored in cells from “leaving” by binding (and ultimately breaking down) the bridges through which iron can flow into the plasma (ferroportin).
Adequate intakes of vitamin D, whose anti-inflammatory properties are well documented, showed a stimulating effect on red blood cell production via reduction of pro-inflammatory molecules.
The anti-inflammatory power of vitamin D may help protect the individual from iron depletion in the following ways ::
- A reduction in pro-inflammatory molecules which reduces hepcidin secretion. Reminder :: high levels of hepcidin makes utilisation of iron difficult or impossible.
- A reduced hepcidin secretion restores iron bioavailability and promotes the production of red blood cells and hemoglobin via restoration of the iron recycling cycle.
- An increased red blood cell production in turn, helps reduce hepcidin secretion, reinforcing the action just described.
Optimal intake of vitamin D acts favorably on iron metabolism in the following ways ::
- Suppresses ARNm transcription of hepcidin.
- Promotes ARNm expression of ferroportin.
Decreased levels of hepcidin and increased presence of ferroportin translates to the improvement of iron recirculation in the body; it increases its availability for hemoglobin and red blood cell production.
In a study published in the Journal of the American Society of Nephrology, healthy volunteers who were administered 100 000IU of a synthetic form of D2 saw their serum levels of hepcidin plummet in 24hrs. Similar results were observed on chronic renal disease patients undergoing dialysis2.
Adequate levels of Vitamin D assists red blood cell production (erythropoïesis) in 2 ways ::
- It triggers BUF-E, Burst-Forming Unit-Erythroïd – proliferation. BUF-E are, in layman’s terms, red blood cell precursors. *Bonus :: BUF-E produce regulators that help to lower hepcidin!
- Vitamin D is a promoter of the hormone responsible for activating red blood cell formation (Erythropoietin)3.
Literature on vitamin D defines its effects a little more each year ::
Yes! Vitamin D is great for bone health… And so much more!
Vitamin D holds important anti-inflammatory properties and supports, directly and indirectly, iron regulation which is of capital importance in red blood cell and hemoglobin production.
In a nutshell , vitamin D in the context of anemia prevention does the following ::
Decreases ::
- Decreases pro-inflammatory molecules that trigger hepcidin secretion
- Decreases hepcidin, which is an inhibitor or iron utilisation
- Decreases erythropoietin resistance; the hormone that stimulates red blood cell production
Increases ::
- Increases serum iron which, available through circulation, can be used and recycled
- Increases production of hemoglobin; an oxygen (and CO2) transporter
- Increases proliferation of erythroid progenitors (BUF-E), red blood cell precursors
- Increases concentration of red blood cells
- Increases erythropoietin secretion
Various studies corroborate these hypotheses :: insufficient intakes of vitamin D in children under the age of 24months4, in the elderly population5, in people suffering from chronic renal disease6 or suffering from cardiac insufficiency7 were all linked to an increased incidence/ risk of anemia. This association is even stronger in the case of inflammatory pathologies such as irritable bowel syndrome, ulcerative colitis, rheumatoid arthritis, Crohn‘s disease et systemic lupus erythematosus8.
Keeping in mind vitamin D synthesized in the skin is only a precursor and requires a 2 step activation process :: first through the liver, second through the kidneys; the vitality of these 2 organs should be taken into account when evaluating your needs.
Healthy individuals should simply aim for adequate intakes; massive doses do not benefit iron metabolism any more than simple “needs are met” quantities.

If you have no clue what your vitamin D recommended intakes are, you can get the info right here. My “VBN – Vitamin D Form” gives details about requirements, sources, depletion interactions and possible risks associated with unnecessary high dosages.
A few studies have been linked through this article, get acquainted with the data if you wish to know more about this topic; this post is merely a quick introduction, a simplified intro into the subject.
Research papers are always a great way to approach a discussion with your health care provider, feel free to share them with yours if you feel it would be useful in the evaluation of your specific needs and the enhancement of your vitality.
Stay curious and humble,
Be well,
Vicky x
** Not discussed here but relevant to circulating vitamin D levels and thus, to the prevention and management of anemia ::
FGF-23 – Inhibitor of kidney conversion of vitamin D. Produced by the kidneys and generally elevated in people suffering from chronic kidney disease.
PTH – Promoter of vitamin D conversion in the kidneys. Produced and regulated in healthy parathyroid glands.
Vicky Bachand ND.A is a naturopath :: a naturopath does NOT replace a medical doctor.
Ideas provided in this article are presented as information only and do not aim to provide in depth details about the chosen topic nor replace the advice of a qualified health care provider.
Information shared here does not constitute a consultation, a diagnosis nor a medical opinion and therefore should not be interpreted as such.
Always consult with your chosen health care provider if you have questions about your personal health.



